How Canada Broke Health Care
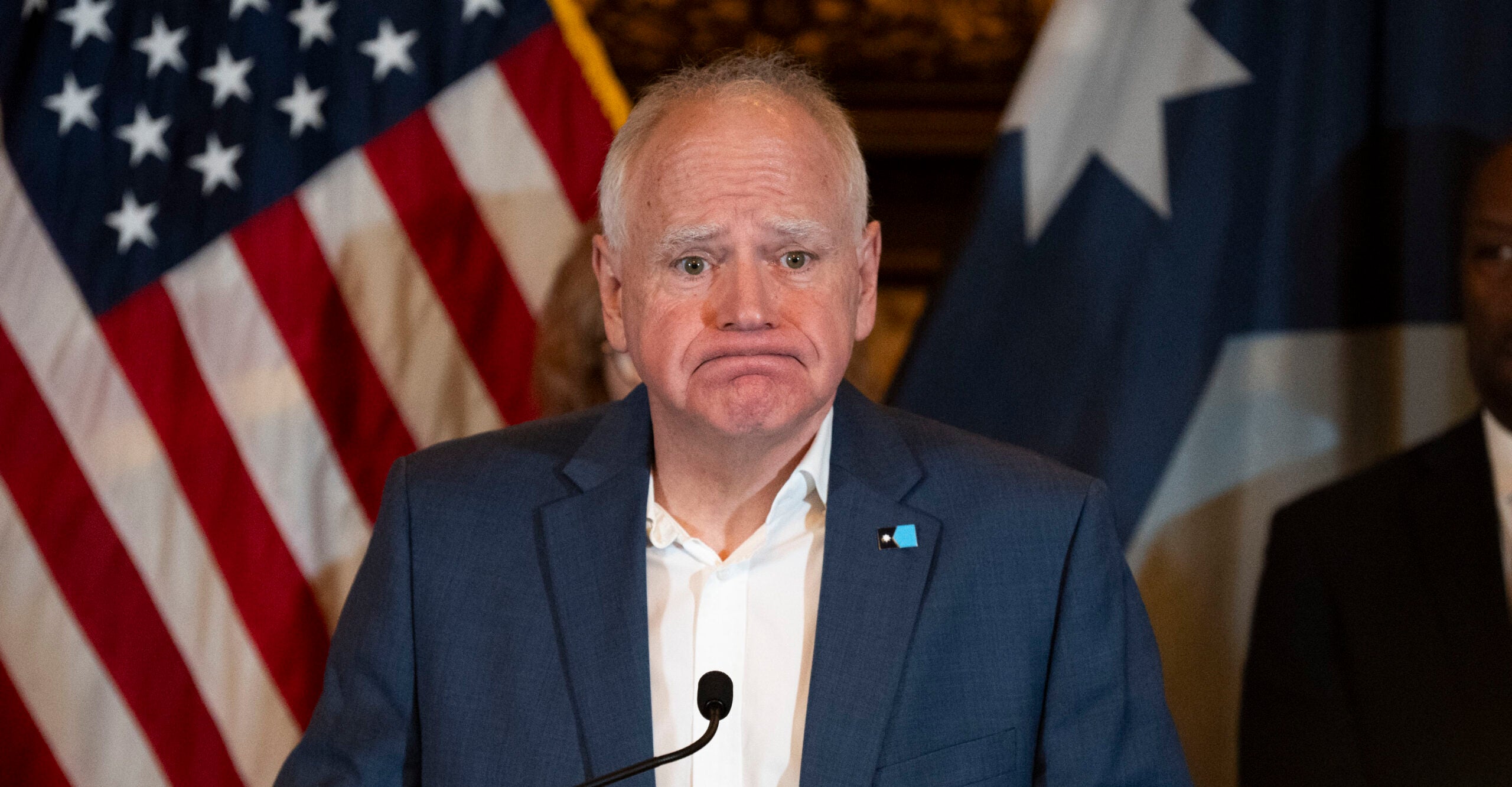
Will provides all the stats to show how Canada’s health care system went from best to busted, and surprise, it wasn’t the Liberal’s fault (well, not mostly).
(0:00 - 1:13) My own recent experience with having secondary cataracts removed got me thinking about our healthcare system, or sick care system if you prefer. Some of you will recall that two years ago I had cataract surgery, a procedure where my eyes' natural lenses were removed and replaced with artificial ones. I left with clear vision and the belief that this meant I couldn't get cataracts again as they can only form on a natural lens. I was wrong. It turns out there's a membrane behind our lens where the same materials that cause the original cataracts can form a new or secondary cataract. Fortunately, that membrane is kind of like our appendix. We don't really need it. When I first started developing cataracts several years ago, the process was so slow I think I probably had them for a couple of years before I noticed that my vision was getting increasingly blurry. The secondary cataracts, however, developed much more quickly. I first started to notice a vision issue last fall, less than a year after my cataract surgery. I thought my eyesight, which has always been very poor, was simply continuing to decline with age. However, by this past spring it became clear that something much more serious was happening. (1:13 - 1:53) I went to see my optometrist and he informed me that I had once again formed cataracts. For those of you unfamiliar with how the 20-20 scale works, someone with 20-20 vision can read from a distance of 20 feet what the average person can read from 20 feet away. By the time I saw my optometrist, my vision had degraded to 2300. This means what the average person could read from 300 feet away, I had to be 20 feet away to read. My optometrist referred me to the Gimbel Eye Center in Calgary, which is where I had my cataract surgery and where I had ICLs implanted when I was 40. If you've never heard of ICLs, I'll explain that in a few minutes. (1:54 - 2:20) The laser procedure to burn away that unnecessary membrane behind my cornea took literally two minutes per eye, with zero recovery time, unless you count waiting for the dilation of my pupils to go down, which did take most of the rest of the day. In addition, the procedure, like my original cataract surgery, was covered by Alberta Health. This seemed logical, since without it I would be functionally blind by now and unable to work and thus pay taxes. (2:21 - 2:30) So covering those procedures is in the government's own interest. The problem was with the wait time. The folks at Gimbel did the best they could. (2:30 - 2:58) I explained that I wasn't retired, that I was in fact still working approximately 70 hours per week, and that my vision had already deteriorated to the point where I could no longer read my teleprompter, like I am right now, and reading my screen was becoming difficult. So they fast-tracked me, which meant waiting three months rather than nine. My optometrist informed me when I saw him that were I American, he could have gotten me into a clinic the same day. (2:58 - 4:55) I don't know what the cost would have been, but I likely would have paid it, rather than continue to struggle daily to maintain a reasonable level of productivity. As it was, by three weeks before the procedure, I could no longer read my screen, at least not without donning reading glasses, leaning in until my face was six inches from the screen and squinting to make out one word at a time. Obviously that was a losing proposition, and that was when I notified you all that I would be doing only the bare minimum until after the procedure, which for those of you who were curious went just fine and I can now see clearly again. Thank you to those of you who expressed your concern. But this brings me to the subject of wait times in Canada. Well, first, some of you are wondering what the heck ICLs are. ICL stands for implanted corrective lens. It's essentially a soft contact lens implanted in my eye to correct my vision. I had this miraculous procedure done when I was 40. At the time, my vision was 2400. On the left is 2020, on the right 2400. And I'd been that way since I was a kid. ICLs are the only option for people like me whose poor vision is so severe that we're not candidates for laser surgery. If I'd had laser surgery as my wife and brother had a few years earlier, my corneas would have ended up so thin that just getting bumped in the eye could have blinded me. The procedure takes about 20 minutes per eye. It's painless and there is zero recovery time. Despite the fact that this was 20 years ago, I can still clearly remember sitting up after the procedure and being able to read the clock on the far side of the room. To put this in perspective for those of you who have never suffered vision problems, my pre-correction vision was so poor that when I took my glasses off at night, I had to make a mental note of where I put them. (4:56 - 5:56) I don't mean on the bedside table. I mean where exactly on the bedside table. Otherwise, the next morning I was feeling around for them with the risk of knocking them to the floor and breaking them. This procedure was, of course, not covered by health care. The cost was $2,000 per eye and worth every penny. Now about those wait times. If you think our health care system, which was once the envy of the world, has been in serious decline for years, you're right. Second Street filed a long list of FOI requests with all provincial governments to find out how many Canadians are dying on surgical and diagnostic waiting lists. According to the data, 75,000 Canadians have died waiting for essential procedures since April 2018, with over 15,000 in 2020 through 2024 alone, the most recent year for which there was up-to-date data. (5:57 - 8:04) But Second Street notes that even that figure is incomplete, as several governments provide either partial data or simply don't track the problem at all. From the data they do have, they estimate that wait list deaths in 2023-2024 were over 28,000. To be fair, some of these people were elderly and likely to die on a waiting list no matter how short it was. Second Street notes that deaths while on waiting lists ran from less than a week to over 14 years in one extreme case. So to be sure things really are getting worse rather than just seeming to, we need to look at year-over-year deaths, and fortunately Second Street was kind enough to provide their data. Only three provinces had historical data sufficient to show a clear picture, B.C., Alberta, and Ontario. For each, you can see that deaths while on waiting lists have climbed consistently since 2015, with some anomalous data during the COVID years due to hospitals basically shutting down and denying essential services and people staying away from hospitals for fear of contracting the deadly COVID virus that's, oh god, going to kill us all. Clearly, however, there is a systemic problem, and more data yet to show it. Length of stay in emergency departments across Canada has also increased dramatically since 2005. Well, actually, I suspect for longer than that, but I don't have data going back more than 20 years. Here's my own research on emergency department wait times for B.C., Alberta, Ontario, and Quebec. Note that some years are estimates due to incomplete data. Here's B.C. The blue bars are admitted patients. 90th percentile means I only used data for the bottom 90% of patients. What this means is that I've cut out the extremely long wait times. This is to show data that is more representative of what the average person should expect to encounter rather than skewing it with experiences that are well out of the ordinary range. The green bars are discharged patients. This means patients who were seen in the emergency department then sent home. (8:04 - 9:24) As you can see, their wait times are much shorter, typically around five to seven hours. For those who were admitted, which is the majority of them, while times varied slightly between the provinces, the charts themselves appear nearly identical, although we can see clearly that it has accelerated substantially since the COVID years. Wait times dropped in 2020 and 2021 due to people staying away from emergency departments. Less patient load, of course, resulted in shorter wait times. But now the 2024 data from last year shows the average wait time in each of these provinces is approaching 50 hours. This means patients sleeping on benches or cots in the halls not being seen by anyone while they wait for assessment. And even when they are admitted, in many cases two days after arriving at the hospital, they still haven't received treatment. All that has changed is they now have a bed in the hospital room rather than in the hallway. We can look at ambulance wait times too, which have also increased in most provinces over the years. But I suspect by now many of you are reaching data overload, so let me give you some figures from my own personal experience. I was a paramedic in Calgary 40 years ago. At that time, the average wait time for an ambulance inside city limits was seven minutes. (9:25 - 10:45) Today it's over 11 minutes. Not too bad considering that Calgary has grown substantially since then. What is significant is the reason for the extra three to four minutes, which is not because the city has grown. Calgary has added 10 new ambulances in recent years to compensate for that growth. The problem is offload wait times at the hospital, which now average 84 minutes. That's almost an hour and a half. When I was a paramedic, we were typically in and out of the hospital in under 20 minutes and back on the street ready for another patient. And even 40 years ago, I had shifts, especially on a weekend night when we left the ambulance hall shortly after our shift started at 5 p.m. and didn't return to the hall until our shift was over at 7 a.m. the next day. As soon as we finished with one patient, we received a call for the next one. And so it went all night. I should note that my experience of not getting back to the hall at all some nights was atypical. I worked at Hall 2 just south of downtown, which is one of the busiest halls in the city. If we were unavailable, Hall 8 was just five minutes further south. I mention that because back then I had never heard the term code red for the ambulance service. Code red means no ambulance is available. (10:45 - 14:26) To be clear, this means every ambulance in the city is out on a call, most of them sitting at the hospital, waiting for hospital staff to sign off and accept responsibility for the patient. And paramedics are not allowed to leave that patient until they do. In recent years, every major city in Canada has experienced code reds, sometimes hundreds of them a year. While we'd like to blame the Liberals and especially Justin Trudeau for this clear degradation of our health care system, the problem has been getting worse since long before Justin's election in 2015. The period from 2005 to 2015 was almost entirely Stephen Harper's Conservative government. So if we can't entirely blame the Liberals, what's going on? Well, quite a lot of things, as it turns out. Public opinion surveys in 2023 showed 40% of Canadians attributed health care issues to inadequate federal funding, up from 26% in 2012. But as with most things, it's not quite that simple. In fact, I've been able to identify eight reasons for the slow-motion collapse of our health care system, which in the end can be bundled into just two reasons. But we'll get to those later. First, we have a breakdown of the federal health care transfer payment system. Significant reductions in federal health care transfers to provinces in the mid-1990s, coupled with provincial austerity measures, destabilized a system accustomed to steady growth. The federal government share of provincial health care funding dropped from approximately 50% in the 1970s to 22% by the 2020s, forcing provinces to manage with constrained budgets. The 1990s saw federal cuts to Canada health transfer payments to the provinces, leading to a real per capita decline in health care spending from 1992 to 1996, a period described as the point of greatest stress for the well, at least until now. These cuts prompted provincial austerity, reducing hospital budgets and services, which had a lasting impact on capacity and access, a problem that's only grown worse since. The reduction in funding led to hospital amalgamations, staff layoffs, and decreased per capita hospital bed capacity by 63% in the 55 years since 1970, exacerbating wait times and limiting access to care. While funding cuts are often blamed, some also argue that mismanagement of existing funds by provinces prioritizing other sectors or inefficient allocation also contributed. In 2000, the federal government changed the system so that provinces could allocate the health transfer payments any way they wanted to. The unconditional nature of federal transfers post-2000 allowed provinces to divert funds away from health care priorities, and they did. This reduction in funds is what has led to a dramatic drop in available beds. Canada's per capita hospital bed capacity has significantly declined since its peak in 1970, dropping from 7 to 2.5 beds per 1,000 people by 2019. This reduction has strained hospital systems, leading to overcrowding and longer emergency department wait times. Ontario's admitted patient wait times rose from 21 hours in 2005 to 48 hours in 2024, partly due to insufficient bed availability. Canada ranks fourth from the bottom among OECD countries in hospital beds per capita, with only Chile, Sweden, and Colombia lower. (14:28 - 14:59) Fewer beds contribute to bottlenecks in emergency departments, as admitted patients cannot be transferred to wards, leading to prolonged emergency department stays and ambulance offload delays. This also increases surgical wait times, as hospital capacity limits elective procedures, contributing to waitlist deaths. The reduction in beds was partly driven by hospital amalgamations in the 1990s intended to cut costs but reducing availability and efficiency. (15:00 - 15:25) Some argue that over-reliance on global budgets, which cap hospital funding regardless of patient volume, disincentivizes hospitals from expanding capacity or treating complex cases. Then there's the mass exodus of doctors from Canada. A severe shortage of family doctors and specialists compounded by burnout and restrictive residency policies has limited access to primary and specialized care. (15:26 - 16:00) Approximately 20% of Canadians lack a family doctor, and 10 million are projected to soon lack primary care access. A 2023 study noted that 30.8% of Quebec residents and 30.9% of Atlantic Canadians lack a primary care provider, with only 35% able to secure same-day or next-day appointments. The Canadian Medical Association reported in 2021 that 48% of physicians screened positive for depression, contributing to retirements and exits from family practice. (16:01 - 16:50) Forty-eight percent. That's nearly half of all doctors in Canada. Residency spots have remained stagnant despite population growth and barriers to licensing foreign-trained doctors exacerbate shortages. Or to put this another way, competition is increasing for a job that pays less and less every year. The shortage drives increased emergency department visits, from 14 million in 2021-22 to 15.1 million in 2022-2023, as patients without primary care seek treatment in emergency rooms, further straining ED wait times. While burnout and retirements are significant, some argue that provincial policies limiting residency spots and slow credentialing of foreign doctors inflate shortages. (16:51 - 18:29) I myself have in the past couple of years met two foreign doctors who couldn't get licensed in Canada. Both spoke clear English and had earned medical degrees in their own countries. Instead of allowing these people to take the exams for Canada and then licensing them if they passed, these two young men were both Uber drivers. Now there's a good use of human resources. Fourth, the current system has a near-total lack of accountability for hospital administrators. Canada's reliance on global budgets for hospitals, where funding is fixed regardless of patient volume, contrasts with activity-based funding models in countries like the Netherlands and Switzerland, which incentivize efficiency. Lack of accountability in federal-provincial funding agreements further complicates reforms. And unlike the Netherlands, where hospitals are paid per service, Canadian hospitals operate under global budgets, treating patients as costs to minimize, leading to inefficiencies and longer wait times. A 2023 CMA analysis found no province met targets for improving primary care access and none tracked emergency department closures, which means patient outcomes for those who visited the emergency room. You heard that right. Hospitals in Canada are not required to report what actually happened to the patients they treated or sent home, which would explain why so many of them were happy to go along with the instructions to tell early-onset COVID patients that there were no effective treatments and to go home and come back when they couldn't breathe. Sending them home cut costs. (18:31 - 19:30) Inefficient funding contributes to long wait times for specialists. 46% of Canadians wait over two months and non-emergency surgeries, where 19.9% wait over a year, while lack of accountability requirements allows provinces to underfund primary care. 5.3% of Canadian health budgets versus 8.1% in other OECD countries. Not surprisingly, critics argue that global budgets prioritize cost control over patient care, while provinces' autonomy in spending federal transfers leads to misallocation. And we still remain one of only three countries in the world with socialized health care that does not allow private practices to directly charge the A practice proven to reduce the load on the public system. Oh, and the other two countries that, like Canada, have socialized medicine but where private practices for essential treatments are not allowed? Yeah, Cuba and North Korea. (19:33 - 21:48) Remember that exodus of doctors? Its effects just keep getting worse. The shortage of family doctors and limited after-hours care have reduced access to primary care, pushing patients toward emergency departments and delaying preventive care, which increases chronic conditions and healthcare costs. In short, in their efforts to save money, our governments, both federal and provincial, have contributed to the problem by making it much harder for people to access healthcare for mild or moderate conditions before they become serious. And most doctors don't work weekends. Only 36% of Canadians have access to care after 5pm or on weekends, and 20% lack a family doctor entirely. So even for those who have a family doctor who, by some miracle, may be able to see them the same day or latest by the following day, that doctor is not available outside of office hours, which means turning to the emergency room, further increasing the load, and that in turn leads to delays in diagnosing conditions, increasing surgical waitlist deaths. For example, 44,273 additional female deaths from 1993 to 2009. And there's a lesson we could take from the UK and Norway where you wouldn't have a doctor, you would have a team of doctors, all of whom would have access to your patient history and any of whom could see you at any time depending upon who was available. And we don't spend money on new tech either, unless you want to count the millions spent by our governments on respirators that killed patients and then were tossed out where scavengers could purchase them for a few hundred bucks each. Canada lags in access to medical technology, ranking second to last in the G20 for MRI units and radiotherapy equipment, and fifth to last for CT scanners with 33% fewer mammography machines than the G20 average. This underinvestment contributes to diagnostic delays, increasing wait times for elective care and surgeries, as noted in the Fraser Institute's report, which recorded the longest surgical wait times in 30 years. And then there was the plandemic, and this one we can blame on Trudeau. (21:49 - 25:36) The plandemic narrative caused people to stay away from hospitals in droves, but that of course only delayed treatment for their conditions. This delay pushed emergency room visits from 14 million in 2021-2022 to 15.1 million in 2022-2023 as patients sought care for untreated conditions, while this backlog contributed to rising surgical wait list deaths and emergency department wait times, while burnout reduced the healthcare workforce, further limiting capacity. And a lot of that burnout came from the fact that vaccine mandates gutted our healthcare system, mostly by firing thousands of nurses and support staff across the country for refusing the vaccines, which meant the load, which had returned to above normal by mid-2022, was now spread across far fewer frontline workers. This is what explains the sharp rise in wait times since 2021. And remember those two weeks to flatten the curve? What actually happened was that the backlog of too-frightened-to-go-to-the-hospital-during-the-plandemic-subsequently-returned-to-a-system-that-had-been-degrading-for-years-and-had-now-had-staff-gutted-by-tyrannical-government-mandates, leaving us with a system which doesn't have anywhere near the capacity to handle the current and growing load, which means it's only going to get worse. And finally, there's the collapse of our economy. A collapse which leads to depressed people eating a poorer diet, not getting any exercise, and thus developing health issues such as diabetes much sooner in life. And because very few of our poor have a family doctor, their health care needs fall disproportionately on our hospitals. I like simple rules though, so those eight factors can be boiled down to really just two things. First, Canada is a socialist country. Socialism lives next door to communism and neither system has ever worked economically. This is because even altruistic socialist governments, if you can bring yourself to believe in such a thing, persist in their delusion that they can look after everyone. In their vain attempts to do so, they ultimately look after no one, while spending obscene amounts of money to do so. Thus, we have one of only three socialized health care systems in the world where we do not have the option of private care. The second reason is this. Fiat currency. A hundred years ago, a dollar was worth a dollar. Today, it's worth three cents. Every fiat currency in history has eventually failed. At this point, over 700 of them. Every single time. Because this has no intrinsic value. And so as inflation and racketeering both government and corporate degrade the agreed-upon value of this dollar, more and more is required to do less and less until the day comes when the dollar is worthless. And this is something that our current liberal government and their globalist masters clearly do understand. In an economic system where the need for resources will always eventually fall victim to a doomed-to-fail currency, the only real long-term solution is to reduce the need for resources. Which is why, in Canada today, you will wait on average for two days to even be admitted through our hospital emergency wards and where you have an ever-increasing likelihood of dying while on a months or even years-long waiting list. But you can get assisted suicide the same day.