How to Protect Patients and Medical Professionals

The Transformation of Medicine: From Healers to Healthcare Workers
I had the privilege of addressing the American Association of Physicians and Surgeons this past Friday at their annual meeting and convention. I spoke on a topic that I’d never addressed publicly before, but one in which I feel quite versed through hard-won experience. During my medical career, which spans four decades, I’ve witnessed profound changes in medicine. But what we’ve seen happen over the past decade isn’t just change—it’s a fundamental transformation that should frighten every American who values quality healthcare.
When I began my career in the 1980s, physicians were truly independent professionals. We owned our practices, made clinical decisions based on our training and experience, and were accountable primarily to our patients and our consciences. The doctor-patient relationship was sacred, protected by both medical ethics and legal precedent. We had time to listen, to think, to develop comprehensive treatment plans tailored to each individual patient.
Today’s reality is starkly different. Physicians are no longer in control of our profession. We’ve witnessed unprecedented interference and control over every facet of medical care, and it’s accelerating at an alarming pace. What troubles me most deeply is not just the external pressures we face, but how these pressures have fundamentally changed the physicians themselves.
I’ve observed a definite decline in the attitude many doctors take toward their patients. There’s a troubling loss of confidence in clinical decision-making and a diminished ability to think critically about disease and illness. Too many physicians have abdicated responsibility for patient outcomes, hiding behind protocols and guidelines rather than taking ownership of their clinical decisions. Perhaps most concerning is the apparent lack of empathy many now show toward a patient’s fundamental right to make informed decisions about their own healthcare.
The transformation is psychological as well as structural. As a profession, many feel a profound loss of authority in directing treatments. Physicians who once confidently prescribed based on their clinical judgment now feel compelled to ask for permission to deviate from standardized guidelines—even when their experience and the patient’s unique circumstances clearly warrant a different approach.
This shift represents more than professional frustration; it’s a betrayal of the trust patients place in us. When I took my oath decades ago, I promised to “First, do no harm.” Today, many physicians find themselves in positions where following institutional protocols may actually harm patients, yet they feel powerless to act on their clinical judgment.
The corporatization of medicine has reduced many physicians from independent professionals to healthcare workers—employees who implement corporate policies rather than medical doctors who heal the sick. Electronic health records have transformed us from healers into data entry clerks. Prior authorization requirements have made us supplicants, begging insurance companies for permission to treat our patients. Quality metrics have reduced the art and science of medicine to checkbox exercises that ignore the complexity of human health and disease.
Perhaps most insidiously, the financial pressures and employment models have created a generation of physicians who have never experienced true clinical independence. They’ve been trained in systems where protocol compliance matters more than patient outcomes, where productivity metrics drive decision-making, and where questioning authority is discouraged or punished.
The Covid-19 pandemic exposed these problems with devastating clarity. Physicians who dared to think independently, who questioned protocols that weren’t working, or who advocated for their patients’ individual needs faced professional destruction. The message was clear: conform or be destroyed.
Yet resistance is not only possible—it’s essential. During my own experience of being terminated for practicing evidence-based medicine and putting patients first, I discovered something profound: liberation from corporate control doesn’t just restore our ability to practice good medicine—it restores our souls as physicians.
The lecture I delivered to AAPS, which I’m sharing below, outlines not just the problems we face, but concrete solutions that are working right now across the country. From Direct Primary Care to pure concierge models, from cash-based specialty services to telemedicine platforms, physicians are finding ways to escape the corporate-government medical complex and return to the practice of real medicine.
The doctor-patient relationship doesn’t have to be a casualty of corporate healthcare. Clinical judgment doesn’t have to be subordinated to insurance company algorithms. Physicians don’t have to be powerless employees implementing someone else’s protocols.
The path back to authentic medical practice requires courage, sacrifice, and commitment to our original oath. It means putting patients before profits, clinical judgment before corporate policies, and medical ethics before financial incentives.
The transformation of medicine from a profession to an industry has been decades in the making. Reversing it will require physicians who remember what we’re supposed to be and patients who demand the care they deserve.
The lecture that follows represents more than an analysis of our current crisis—it’s a blueprint for reclaiming our profession and restoring the sacred trust between doctor and patient that has been the foundation of healing for millennia.
The choice is ours. We can continue as healthcare workers implementing corporate protocols, or we can reclaim our identity as physicians dedicated to healing the sick, one patient at a time.
Introduction
Good afternoon, colleagues. Today we gather at a critical juncture in American medicine—a time when the fundamental principles that have guided our profession for centuries are under unprecedented assault. The sacred doctor-patient relationship, the cornerstone of healing, is being systematically dismantled by forces that view healthcare not as a calling to heal, but as a commodity to be controlled and monetized.
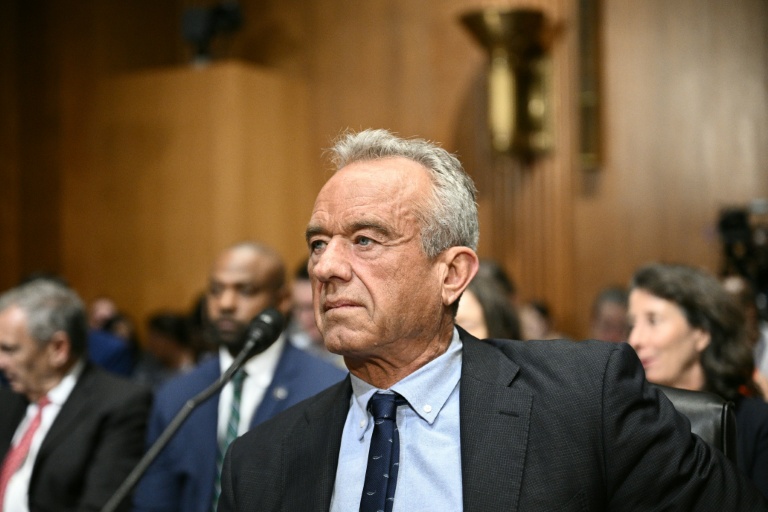
I’m Dr. Brooke Miller, a family physician from Washington, Virginia…a small town approximately 50 miles southwest of here. Along with my wife Ann, we own Miller Family Health & Wellness, a primary care practice focused on acute care, prevention, and reversal of chronic disease. We also operate a purebred Angus cattle ranch, which I’ve been involved in my entire life.
While these two businesses appear vastly different, they share a troubling commonality—both have been severely damaged by centralized corporate control. In agriculture, four multinational beef packing corporations have destroyed free market competition in the cattle market…Their monopolistic practices have forced countless ranchers out of business, creating a crisis in America that threatens our nation’s food security. The parallels to what we’ve witnessed in medicine are striking and sobering.
In medicine, we’ve seen the same pattern of corporate centralized control that has systematically destroyed the doctor-patient relationship. In 2020, like many physicians across this country, I was employed by a healthcare corporation. Instead of the freedom to follow my medical training and clinical judgment in treating patients, I faced enormous pressure to follow corporate policies that I fundamentally disagreed with based on evolving scientific evidence.
When I publicly spoke out against mask mandates, I was effectively placed under a gag order. Corporate administrators—not physicians—attempted to dictate what I could and could not say about medical matters. Despite this pressure, I followed my conscience and my oath. I treated each patient individually with repurposed medications, vitamins, and nutraceuticals, combined with diet and lifestyle recommendations—all based on my clinical knowledge and the emerging evidence. This approach was successful, with excellent outcomes.
For practicing evidence-based medicine and putting my patients’ individual needs above corporate protocols, I was fired from my position. Today, I proudly proclaim that being terminated was one of the most positive things that could have happened to me. It freed me from bondage to practice medicine and follow my oath—where each patient in front of me is treated as a unique individual with individual needs, not as a statistic in a corporate algorithm.
This experience opened my eyes to the broader systematic assault on medical freedom and physician autonomy that threatens not just individual doctors, but the very foundation of quality patient care in America.
The erosion of medical independence didn’t happen overnight. It has been a gradual…but deliberate process, accelerated dramatically during recent years, where financial incentives, regulatory mandates, and corporate control have displaced clinical judgment and patient welfare as the driving forces in healthcare delivery. Today, I will examine how government interference and corporate medicine are violating medical ethics, destroying physician autonomy, and harming patient care.
Government Interference in Medical Practice
The government’s intrusion into medical practice has created a system where bureaucrats, not physicians, increasingly dictate patient care. This interference manifests in several destructive ways.
Financial Coercion through Federal Programs
Medicare and Medicaid, originally designed as safety nets, have become tools of control. Quality metrics tied to reimbursement force physicians into one-size-fits-all protocols that ignore individual patient needs. A diabetic patient with unique circumstances must be treated according to standardized algorithms, not clinical judgment, if the physician wants to avoid financial penalties.
Prior authorization systems represent perhaps the most egregious violation of the doctor-patient relationship. Insurance companies, backed by government programs, now routinely override physician prescriptions….Emergency medications are delayed while patients suffer. Life-saving procedures are postponed pending bureaucratic approval. The system prioritizes cost containment and insurance company profit over clinical necessity, transforming physicians from healers into supplicants begging for permission to treat their patients.
Meaningful Use requirements have turned physicians into data entry clerks. Electronic health records, mandated and subsidized by government programs, prioritize data collection for regulatory compliance over patient care. Physicians spend more time clicking boxes on computer screens than examining patients, destroying the human connection that is essential in our profession.
Regulatory Mandates and Clinical Suppression
Government agencies increasingly practice medicine without licenses. Protocol-driven medicine, enforced through regulatory pressure and financial incentives, treats patients as statistical averages rather than unique individuals…Physicians who deviate from approved protocols—even when clinical judgment support alternatives—face investigation, censure, and loss of livelihood.
State medical boards, influenced by federal guidance and pharmaceutical industry pressure, have become instruments of intimidation rather than professional oversight. Off-label prescribing, a cornerstone of personalized medicine for decades, is now viewed with suspicion. Pharmacists routinely question and sometimes refuse to fill prescriptions harming patient care.
The suppression of medical free speech has reached alarming proportions. Physicians who question official narratives or share clinical observations that contradict approved messaging face censorship, professional sanctions, and career destruction. This climate of fear stifles scientific inquiry and prevents the open discourse essential to medical progress.
The Covid-19 Case Study: CARES Act Perverse Incentives
The Covid-19 pandemic exposed the dangers of government control over medicine with devastating clarity. The CARES Act created a system of perverse financial incentives that prioritized profit over patient lives.
Hospitals received bonus payments for Covid-19 diagnoses, creating powerful incentives to label patients as Covid-positive regardless of clinical presentation. Remdesivir, despite questionable efficacy and harmful side effects, became the mandated treatment because it generated substantial reimbursements. Ventilator protocols, supported by financial incentives, were implemented even when clinical evidence demonstrated harm.
These financial manipulations created a system where hospitals profited from following protocols rather than achieving positive outcomes. Physicians who questioned these approaches or used alternatives faced immediate retaliation. An example of such tyranny is here with us today…He is an innovator and hero who saved countless lives not only in his ICU, but also through his contribution to treatment strategies, inspiring me….as well as countless providers all over the world. Thank you, Dr. Paul Marik! Please give him a hand!
This medical system served financial interests rather than patient welfare, dehumanizing patients and violating every principle of medical ethics. Yet Paul, as well as many courageous physicians and nurses all over the world resisted this madness and fought back.
Corporate Medicine’s Control Mechanisms
Employment-Based Control Systems
Hospital acquisition of physician practices has concentrated healthcare delivery in the hands of large corporations. The Corporate-employment model has fundamentally altered the practice of medicine and destroyed physician autonomy. Doctors, once independent professionals accountable to their patients exercising clinical experience and judgment, have become employees accountable to corporate supervisors and protocols. This cookie-cutter approach to medicine ignores the reality that each patient is unique.
Productivity metrics based on RVUs. (I despise those letters) prioritize volume over quality, incentivizing quick encounters rather than quality care.
Corporate committees, staffed by administrators and physicians who have abandoned clinical practice, now routinely override physician decisions. Treatment recommendations are filtered through cost-benefit analyses that prioritize corporate profit margins over patient outcomes. Non-compete clauses trap physicians in employment arrangements while preventing them from maintaining relationships with their patients.
Insurance Company Interference
Insurance companies have inserted themselves between physicians and patients, creating barriers to timely and appropriate care. Prior authorization requirements are burdensome and often delay treatment. Formulary restrictions force patients to use inferior medications based on cost considerations rather than clinical efficacy.
Step therapy requirements mandate that patients fail on cheaper, often inferior treatments before accessing more effective options. This approach prolongs suffering and often increases total healthcare costs while generating profits for insurance companies. The physician becomes a mere functionary in this system, implementing corporate decisions rather than exercising medical judgment.
Violations of Medical Ethics and Patient Rights
These government and corporate intrusions represent fundamental violations of medical ethics that have guided our profession since Hippocrates.
Informed Consent Erosion
True informed consent requires that patients receive complete information about treatment options, risks, and benefits. Government and corporate pressures systematically undermine this process. Physicians are prevented from discussing alternative treatments that deviate from approved protocols. Patients receive incomplete information because their physicians fear retaliation for honest discussions.
Emergency use authorizations and mandated treatments have further eroded informed consent. Patients are pressured into accepting treatments without full disclosure of risks or alternatives. The coercive environment created by government mandates and corporate policies makes truly voluntary consent impossible.
Breaches of Doctor-Patient Confidentiality
Government health databases collect private medical information without meaningful patient consent. Corporate data mining exploits patient information for profit while patients remain unaware of how their most private information is being used.
These violations destroy the trust essential to the doctor-patient relationship. Patients become reluctant to share sensitive information when they know it will be stored in government databases or sold to corporate interests. The result is inferior medical care based on incomplete information.
Practical Solutions and Alternatives
Despite these challenges, solutions exist that can restore medical autonomy and improve patient care. These alternatives require courage and commitment but offer hope for preserving the medical profession’s integrity.
Direct Primary Care Model
Direct Primary Care represents a return to the fundamental doctor-patient relationship. By eliminating insurance middlemen through monthly membership fees, DPC restores physician independence and improves patient care. Physicians in DPC practices report higher job satisfaction, lower burnout rates, and better patient relationships.
DPC patients receive more time with their physicians, same-day appointments, and direct access to their doctors. Transparent pricing eliminates surprise bills and gives patients control over their healthcare spending. Most importantly, DPC physicians have the clinical freedom to practice evidence-based medicine without external interference.
Studies consistently show that DPC practices achieve better outcomes at lower costs. Chronic disease management improves when physicians have time to develop comprehensive treatment plans. Emergency room visits decrease when patients have ready access to their primary care physicians. The model proves that removing bureaucratic interference improves both patient satisfaction and clinical outcomes.
Concierge Medicine
Concierge medicine also offers an alternative to traditional practices.
Patients pay an annual membership fee—typically ranging from $1,500 to $5,000. This membership fee provides enhanced services, including longer appointment times, same-day or next-day access, 24/7 physician availability, and smaller patient panels that allow for more personalized attention. The physician continues to bill insurance companies for all covered medical services and procedures.
Concierge care offers improved doctor-patient relationships, unhurried appointments and higher overall patient and doctor satisfaction.
Cash-Based Specialty Services
Ambulatory surgery centers, imaging facilities, and laboratory services that operate on a cash-pay basis consistently deliver high quality care at lower costs than hospital-based services. These facilities eliminate administrative overhead and focus on clinical excellence rather than regulatory compliance.
Patients benefit from transparent pricing, shorter wait times, and personalized service. Physicians in these facilities report higher satisfaction because they can focus on patient care rather than bureaucratic requirements. The success of these cash-based services demonstrates that removing government and insurance company interference improves both quality and affordability.
Legal and Advocacy Solutions
Protecting medical freedom requires active advocacy and legal reform. Medical freedom legislation at the state level can protect physicians who practice evidence-based medicine from disciplinary action. Professional liability reform should protect physicians who follow clinical judgment rather than corporate protocols.
Transparency requirements should mandate disclosure of financial incentives that influence medical recommendations. Patients have the right to know when their physicians’ treatment recommendations are influenced by government payments or corporate bonuses.
Call to Action and Conclusion
The path forward requires individual action and collective commitment to medical freedom. Each physician must consider how to practice medicine according to ethical principles rather than corporate mandates. For many, this may mean transitioning to direct-pay models that eliminate third-party interference in the doctor-patient relationship.
We must advocate for medical freedom at every level—local, state, and national. Professional organizations that truly represent physician interests, rather than corporate healthcare systems, deserve our support. We must speak out against policies that prioritize bureaucratic control over patient welfare, even when doing so requires personal sacrifice.
Individual Physician Actions
Consider transitioning to practice models that restore physician autonomy—Direct Primary Care, concierge medicine, or cash-based specialty services. Support legislation that protects medical freedom and opposes measures that increase government control over medical practice. Join organizations like AAPS that advocate for physician independence rather than corporate interests.
Most importantly, remember your oath to do no harm and put patient welfare above all else. The courage to practice ethical medicine, even when it conflicts with government mandates or corporate policies, is what distinguishes true healers from those who prioritize institutional compliance over patient welfare.
Systemic Changes Needed
We must work toward fundamental reform that separates medicine from government control. Healthcare should be a private matter between physicians and patients, not a public utility managed by bureaucrats. True informed consent must be restored, with physicians free to discuss all treatment options without fear of reprisal.
The doctor-patient relationship must be protected from corporate interference. Employment contracts that restrict physician judgment should be challenged. Non-compete clauses that prevent physicians from maintaining patient relationships must be eliminated.
Final Thoughts
The practice of medicine has survived plagues, wars, and countless challenges throughout history because physicians have remained committed to their patients. Today’s challenges are different but not insurmountable. The principles that have guided our profession—primum non nocere, patient autonomy, informed consent, and the sanctity of the doctor-patient relationship—remain our BEACON.
Corporate and government control over medicine is not inevitable. It exists because we have allowed it to exist. By returning to practice models that prioritize patients over profits and clinical judgment over bureaucratic compliance, we can restore the integrity of our profession.
The patients we serve deserve physicians who are free to practice evidence-based medicine without corporate or government interference. They deserve doctors who have time to listen, to examine, and to heal. They deserve the full truth about their treatment options, not filtered information designed to serve someone else’s financial interests.
The future of medicine depends on our willingness to defend these principles, even when doing so requires personal sacrifice. The doctor-patient relationship is sacred, and it is our responsibility to protect it for future generations of physicians and the patients we are privileged to serve.
Humanity is counting on us. We must not fail.
Thank you.
Republished from the author’s Substack
-

Dr. Brooke Miller is a physician, rancher, past president of the United States Cattlemen’s Association, and advocate for agricultural safety and public health.
Recent Top Stories
Sorry, we couldn't find any posts. Please try a different search.