Did Covid Vaccines Really Save Millions?

[This article was co-authored by Yaffa Shir-Raz, Shay Zakov, and Peter A. McCullough.]
Two years have passed since the official end of the Covid-19 pandemic, yet the topic of vaccination remains highly sensitive in both public and scientific discourse. Attempts to question the legitimacy of the mass vaccination campaign or to raise concerns about potential harms are often met with a moral red line: the widely repeated claim that “Covid-19 vaccines have saved millions and millions of lives.”
Remarkably, this assertion was treated as established fact even during the recent U.S. Senate PSI hearing on May 21, 2025, which focused on vaccine-related adverse outcomes.1 Ranking Member Richard Blumenthal opened the hearing with the following statement:
“As we talk about the side effects of COVID vaccines, I think we need to be clear about the most important fact. For all Americans, COVID-19 vaccines have saved millions and millions of lives. There is no scientific question about that fact…One study found that 3 million American deaths were averted…in the United States…I would like this study entered into the record.1
This confident assertion raises a fundamental question: Is there truly solid and conclusive scientific evidence to support the powerful claim that the Covid-19 mass vaccination campaign resulted in a net benefit of millions of lives saved?
Faced with this fundamental question, our research team undertook a structured, step-by-step evaluation of the empirical foundations of the “millions saved” narrative. Building on our prior work,2, 3 we critically examined the hypothetical statistical models that produced this extraordinary figure, as well as multiple randomized controlled trials and large-scale observational studies that served as the empirical basis for the vaccine efficacy estimates fed into these models.
We have now uploaded our full-length article with what we believe to be urgently important findings to a preprint server,4 in order to allow scientists, physicians, and policymakers to independently evaluate the evidence. Because meaningful scientific discourse requires careful scrutiny of the data, we strongly urge readers not to rely solely on the current brief article, but to engage directly with the full analysis presented in our preprint.4
Our goal here is to highlight several central findings that, in our view, demand serious attention, given their direct relevance to one of the most significant public health interventions in modern history: a global, government-backed mass vaccination campaign that, in many countries, was accompanied by mandates and unprecedented restrictions on individual freedoms.
What follows is a concise overview of key insights from our structured analysis that, in our view, every health professional, policymaker, and citizen deserves to consider:
- The widely cited claim that “millions of lives were saved” by Covid-19 vaccines is based on hypothetical models that rest on a long sequence of assumptions—many of which are either weak, unvalidated, or demonstrably false (see below). As a result, the outputs of these models are of questionable value and cannot be taken as reliable evidence.
- A central assumption underlying these models was that Covid-19 vaccines provided strong and durable protection against infection and transmission. Consider the original statement by Dr. Anthony Fauci, then Chief Medical Advisor to the US President: “When you get vaccinated you not only protect your own health…but also you contribute to the community health by preventing the spread of the virus throughout the community…you become a dead end to the virus” (bold added).5 This assumption—serving as the cornerstone of the mass vaccination campaign—turned out to be false. Real-world data quickly revealed that vaccine efficacy against infection was fragile and short-lived, and efficacy against transmission was never directly studied.
- Strikingly, despite the collapse of this original narrative (point 2), the vaccination campaign continued under a revised justification: that the vaccines provide lasting protection against severe illness and death, even after their short-term effect against infection diminishes. It is important to recognize that this updated claim hinges on a conceptual separation between these two types of efficacy—a separation that, as we demonstrate repeatedly in our preprint article, was never empirically validated.
- In fact, available data suggest that protection against infection and protection against severe illness or death are closely linked, following a similar trajectory of waning over time. The difference lies primarily in timing, with a natural delay between initial infection and the development of severe outcomes.
- To directly assess the validity of this supposed distinction between protection against infection and protection against severe illness, we examined the conditional probability of severe illness among individuals who became infected across several key studies. The results were clear: the apparent protection against severe outcomes was most likely a byproduct of the short-term protection against infection. None of the influential studies we analyzed demonstrated independent or durable protection against severe illness or death.
- Notably, some studies stopped tracking severe outcomes precisely at the point when vaccine protection would be expected to wane—paralleling the well-documented decline in protection against infection and the typical delay between infection and the onset of severe illness or death mentioned above. This pattern raises serious concerns about potential misrepresentation or selective reporting of research findings.
- Finally, the pivotal randomized controlled trial that led to the Emergency Use Authorization (EUA) of the Pfizer vaccine showed no meaningful difference between the vaccine and placebo groups in preventing: (1) flu-like symptoms, (2) severe Covid-19, or (3) all-cause mortality. The only significant difference was observed in a non-clinical outcome—laboratory-confirmed Covid-19 infection—and even this result was based on data from no more than 8.24% of participants, collected in a potentially biased manner, as detailed in our preprint.
- Notably, no Covid-19-related deaths were recorded in Pfizer’s pivotal trial. This absence raises serious questions about whether the legal and medical criteria for issuing an emergency use authorization were truly met.
- Even more importantly, the six-month follow-up trial by Pfizer reported 15 deaths in the vaccine group (n = 21,720), compared to 14 in the placebo group (n = 21,728). Given the large sample size, this lack of mortality benefit should have served as a critical anchor for any hypothetical model or evidence-based discussion regarding the overall benefit of the vaccine.
These findings seriously challenge the notion that Covid-19 vaccines saved millions of lives. Moreover, our in-depth investigation uncovered a broader range of methodological flaws that cast doubt on the overall reliability of the existing evidence base. These include: (a) followup periods that were exceedingly short and inconsistently applied across groups; (b) implausible efficacy signals appearing almost immediately after vaccination—well before full immunization could have occurred biologically; and (c) heavy reliance on observational data vulnerable to Healthy Vaccinee Bias, differential testing rates, and numerous other confounding factors.
Taken together, these methodological and empirical concerns not only undermine the foundation of the “millions saved” narrative, but also raise a deeper question: If the evidence is so limited and flawed, how did this narrative gain such dominance in scientific and public discourse?
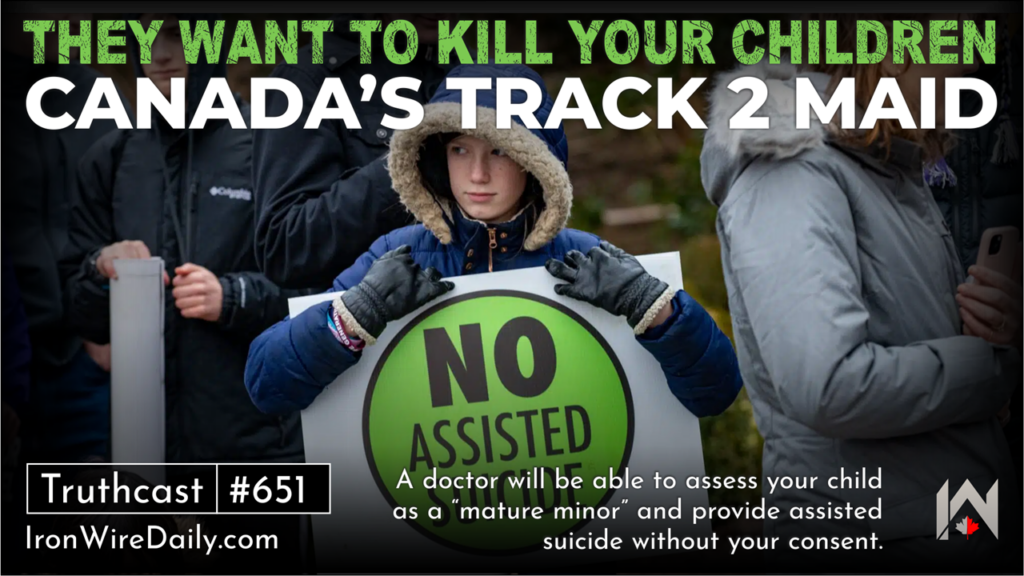
The issue is not whether some degree of vaccine efficacy was observed at specific moments (e.g., see the fascinating example in our preprint of the Bar-On et al. study on the second booster), but rather how such fleeting observations came to shape the broader public narrative. Isolated data points were elevated and decontextualized, while critical considerations—such as (a) waning immunity, (b) the lack of demonstrated mortality benefit, (c) vaccine breakthrough infections leading to hospitalization or death, and (d) an increasingly robust body of evidence on adverse effects—were systematically sidelined (Figure 1).
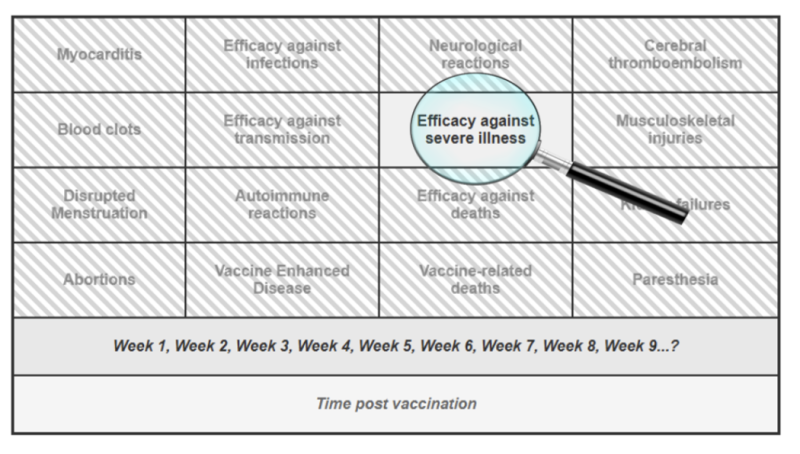
This narrowing of focus — peering through the keyhole of one transient success — has allowed a fragile claim to solidify into a powerful myth, reinforced by institutional authority, social conformity, and the systematic suppression of dissenting voices (including our own experience of censorship, as detailed in our preprint).
We therefore call on the scientific and medical communities to take a step back, widen the lens, and return to a foundational principle of medicine: every intervention, no matter how promising, must undergo continuous, evidence-based evaluation of both its benefits and its potential harms. To the best of our knowledge, such a balanced and rigorous appraisal has yet to be applied to the Covid-19 vaccines.
Based on the evidence reviewed in our preprint, we conclude that the claim that “Covid-19 vaccines saved millions and millions of lives”1 is not supported by empirical evidence. While these vaccines were widely promoted as safe and effective, accumulating reports of serious adverse events—such as myocarditis, pericarditis, thrombosis, and neurological symptoms—have been extensively documented across pharmacovigilance systems and in multiple peer-reviewed studies (e.g., 6-16), many co-authored by the last author of the current article.
Notably, this biologically active intervention was administered repeatedly in the form of boosters, thereby compounding potential risks—often in populations with near-zero risk of Covid-related mortality, such as children. Taken together with the lack of demonstrable long-term efficacy presented in our preprint,4 the available evidence suggests that the risk–benefit balance of the Covid-19 vaccines may, in fact, tilt toward the negative end of this fundamental medical equation.17, 18
References
1. Homeland Security. The Corruption of Science and Federal Health Agencies: How Health Officials Downplayed and Hid Myocarditis and Other Adverse Events Associated with the COVID-19 Vaccines.
2. Ophir Y, Shir-Raz Y, Zakov S, McCullough PA. The Efficacy of COVID-19 Vaccine Boosters against Severe Illness and Deaths: Scientific Fact or Wishful Myth?. Journal of American Physicians and Surgeons. 2023;28(1). doi: https://www.jpands.org/vol28no1/ophir.pdf.
3. Ophir Y. The Final Brick in the Vaccine Efficacy Narrative ⋆ Brownstone Institute. 2023.
4. Ophir Y, Shir-Raz Y, Zakov S, McCullough PA. A Step-by-Step Evaluation of the Claim That COVID-19 Vaccines Saved Millions of Lives. Researchgate (preprint). 2025. doi: 10.13140/RG.2.2.12897.42085.
5. NEWS C. Transcript: Dr. Anthony Fauci on “Face the Nation,” May 16, 2021. 2021.
6. Rose J. A Report on the US Vaccine Adverse Events Reporting System (VAERS) of the COVID-1 9 Messenger Ribonucleic Acid (mRNA) Biologicals. Science, Public Health Policy, and The Law. 2021;2:59–80.
7. Fraiman J, Erviti J, Jones M, et al. Serious adverse events of special interest following mRNA COVID-19 vaccination in randomized trials in adults. Vaccine. 2022;40(40):5798–5805. doi: 10.1016/j.vaccine.2022.08.036.
8. Shir-Raz Y. Breaking: Leaked Video Reveals Serious Side-Effects Related to the Pfizer COVID-19 Vaccine Covered Up by the Israeli MOH. 2022.
9. Witberg G, Barda N, Hoss S, et al. Myocarditis after Covid-19 Vaccination in a Large Health Care Organization. N Engl J Med. 2021;385(23):2132–2139. doi: 10.1056/NEJMoa2110737.
10. Chua GT, Kwan MYW, Chui CSL, et al. Epidemiology of Acute Myocarditis/Pericarditis in Hong Kong Adolescents Following Comirnaty Vaccination. Clinical Infectious Diseases. 2021:ciab989. doi: 10.1093/cid/ciab989.
11. Hulscher N, Alexander PE, Amerling R, et al. A Systematic REVIEW of Autopsy findings in deaths after covid-19 vaccination. Forensic Sci Int. 2024:112115. doi: 10.1016/j.forsciint.2024.112115.
12. Oster ME, Shay DK, Su JR, et al. Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021. JAMA. 2022;327(4):331–340. doi: 10.1001/jama.2021.24110.
13. Takada K, Taguchi K, Samura M, et al. SARS-CoV-2 mRNA vaccine-related myocarditis and pericarditis: An analysis of the Japanese Adverse Drug Event Report database. Journal of Infection and Chemotherapy. 2024.
14. McCullough P, Rogers C, Cosgrove K, et al. Association between COVID-19 Vaccination and Neuropsychiatric Conditions. 2025.
15. McCullough PA, Hulscher N. Risk stratification for future cardiac arrest after COVID-19 vaccination. World J Cardiol. 2025;17(2):103909. doi: 10.4330/wjc.v17.i2.103909.
16. Hulscher N, Hodkinson R, Makis W, McCullough PA. Autopsy findings in cases of fatal COVID-19 vaccine-induced myocarditis. ESC Heart Failure. 2024;n/a. doi: 10.1002/ehf2.14680.
17. Mead MN, Seneff S, Wolfinger R, et al. COVID-19 Modified mRNA “Vaccines”: Lessons Learned from Clinical Trials, Mass Vaccination, and the Bio-Pharmaceutical Complex, Part 1. International Journal of Vaccine Theory, Practice, and Research. 2024;3(2):1112–1178. doi: 10.56098/fdrasy50.
18. Mead MN, Seneff S, Rose J, Wolfinger R, Hulscher N, McCullough PA. COVID-19 Modified mRNA “Vaccines”: Lessons Learned from Clinical Trials, Mass Vaccination, and the Bio-Pharmaceutical Complex, Part 2. International Journal of Vaccine Theory, Practice, and Research. 2024;3(2):1275–1344. doi: 10.56098/w66wjg87.
-

Dr. Yaakov Ophir is Head of the Mental Health Innovation and Ethics Lab at Ariel University and a member of the Steering Committee for the Centre for Human-Inspired Artificial Intelligence (CHIA) at the University of Cambridge. His research explores digital-age psychopathology, AI and VR screening and interventions, and critical psychiatry. His recent book, ADHD Is Not an Illness and Ritalin Is Not a Cure, challenges the dominant biomedical paradigm in psychiatry. As part of his broader commitment to responsible innovation and scientific integrity, Dr. Ophir critically assesses scientific studies related to mental health and medical practice, with particular attention to ethical concerns and the influence of industrial interests. He is also a licensed clinical psychologist specializing in child and family therapy.